
BLOOD VOLUME in ME
by Dr David Bell
II. Blood volume in ME
MAST T experiment
During a recent lecture I mentioned some old data concerning blood volume. I was asked to put my thoughts and what I had said on paper. Although it is not new information (the first ME blood volume paper was in 19511) I think it is still an important piece of the puzzle. The first slide is a description of what is meant by low blood volume as distinct from anemia.

In this slide, imagine three buckets and in each is all the blood of three different persons. The first is a healthy person with roughly five quarts of blood divided into two portions, the red blood cells which carry oxygen and the plasma. The second is a person with anemia. In this person the total volume of blood is normal, but the proportion is not. In anemia, the red cells are reduced compared to normal, and this reduction causes fatigue. In the third bucket, a person with ME has low blood volume, but the proportion of red blood cells and plasma is normal. The accumulated volume, instead of being five quarts is down to three or four quarts.
In the first study of blood volume in ME, eighty percent of ME patients were abnormal compared to historical controls1. This was subsequently confirmed by a study out of Miami2. In addition, the volume has been studied in POTS which can co-exist with ME in up to 40%3. And the blood volume can be strikingly low.
Let us put this in context. If a person loses 25% of his or her blood in a car accident, it can be fatal. But the body’s mechanism of anti-diuretic hormone, shunting, and other mechanisms can correct the blood loss quickly. In ME, these mechanisms are not at work, something that has caused me many sleepless nights.
The measurement of blood volume is rarely done now. The most accurate test is the Chromium51 assay. In this test, done in the nuclear medicine department of a University hospital, a tube of blood is drawn from the patient, carried into the back room and the red blood cells are labeled with Chromium51. The Albumin in the plasma portion is labeled with Albumin 125 and the blood is re-injected back into the patient. After an hour or so the labeled blood is mixed thoroughly with the rest of the patient’s blood, and another tube of blood is drawn and carried into the back room. There the amount of Chromium51 and Albumin 125 are measured. By calculating with the patient’s weight, a very accurate determination of the blood volume is made. A newer test, the Daxor BVA-100 (Blood Volume Analyzer) is similar, although I have not yet seen results from ME patients as yet.
The Chromium51 test was devised in the 1960’s to see how much fluid a clinician should remove with diuretics in hypertension and congestive heart failure. The test is not needed for this now, but it was said that with this test you could predict who lived at the bottom of a mountain and who lived at the top. (At the top you need more blood because the air is thin). Some people have said the blood volume reduction is no big deal because astronauts get it. But their reduction is in the 15% range. It is caused by the lack of gravity permitting the blood flow throughout the body to increase, and the kidneys, a little confused, get rid of what they see as the ‘extra’ fluid.
A few years ago, a woman astronaut who had been in the space station for a while returned to earth and gave a short interview to the press. During this interview she collapsed and had to be helped off the podium. Her volume was about 83% of normal due to her time in space. After returning to earth about a quart of blood went into her legs because of gravity while standing and this caused such a drop in cerebral blood flow that she became syncopal. And she had a small drop in volume. In contrast, ME patients have a volume that can be as low as 50% of normal.
There are several mechanisms that come into play when the blood volume falls. The first is the hormone ADH (anti-diuretic hormone) which is missing in diabetes insipidus (not sugar diabetes or diabetes mellitus). In diabetes insipidus an injury or tumor of the pituitary causes ADH production to halt and persons with this condition urinate a great deal and carry around water jugs with ice water (sound familiar?) There have been a number of studies on DI and ADH and without going into details, ADH can be produced in persons with ME hypovolemia. It is just that the pituitary does not seem to think that the hypovolemia is wrong or bad, no big deal. However something recognizes it as a big deal because people with ME can drink up to three gallons of water daily. When I asked an endocrinologist about this, he said it was ‘psychogenic water drinking.’
After wrestling with this problem for many years, the only explanation I can come up with is that the cumulative sum of blood vessel diameter is reduced. The pipes are smaller than they should be. This would mean that the body has re-adjusted to the decreased flow of blood. Part of the adjustment is to shunt blood to the heart, lungs and kidneys and avoid the brain. An excellent theory would be that there is an autoimmunity4 to something that regulates blood vessel size, and this decreases both circulating blood volume and cerebral blood flow5, 6. The amount of autoimmune vasoconstriction would not need to be great as there are many miles of blood vessels in the body.
One reason I favor this theory is that with the administration of one liter of normal saline can nearly reverse the symptoms of ME in about three quarters of patients. This effect, however, wears off within 24 hours and then everything reverts to the newly established normal decreased flow. A similar mechanism may be at play in septic shock, where, at a certain point, even with antibiotics and fluids, the mechanism causing the shock cannot be reversed.
However, and this point is very controversial, I saw two adolescents with two to three months of typical ME (note that it cannot be diagnosed until six months of symptoms have elapsed) and gave them saline infusions daily for a week. For both adolescents, the symptoms they had disappeared never to return, although I have not had contact with them now for several years. Prior to these two adolescents, I saw many ME patients who had the illness at three months, and all stayed ill past the six month mark. If this is true, then early recognition may offer a way to avoid full ME. This material cannot be published because it is so speculative, but if I had a child or relative with what looked like early ME, I would certainly give IV saline.
IV saline was a treatment I used for 22 adults with ME. As mentioned previously, 20% of ME patients had a volume above 80% of normal, and IV saline did not help them. Ironically, they were the most ill of the patients I treated. When I tried to infuse saline they had to stop after about 200 cc’s. From what they said, I could imagine that their cerebral circulation was so constricted that trying to force more fluid into the vessels could not be tolerated. But, there has been almost no research in this area.
Now, the even more drastic treatment, blood transfusion. Many years ago I published a book online called Faces of CFS. In this book I described a woman with very severe ME who had a blood transfusion. About six week before this episode, she had a standard blood volume test which showed her to have about 64% of normal blood volume. She had been feeling ill one day and had ingested two gallows of water or other liquids. Then, probably because she took too many ibuprofen tablets, she vomited blood. At the emergency ward, a hematocrit (Hct) showed anemia, due to a low volume to start then diluted with two gallons of water. I don’t think the vomiting blood contributed anything. But she was given two units of packed cells to be on the safe side.
The next day she felt wonderful; she felt ‘almost normal’, the first time she had said that in the years I had known her. Because she had been a nurse at the local hospital, she saw a hematologist who took her on. After about six weeks she gradually began to decline back to where she had been prior to the transfusion. After a few weeks of decline, the hematologist gave her another transfusion, and again she felt well. This continued for many months until the hematologist said he could no longer give the transfusions because of the risk of her developing allergic reactions to them.
Many years ago there was a condition called ‘idiopathic hypovolemia’, a condition diagnosed by a low blood volume that no one could explain7. Some hematologists treated it with blood transfusion with good results. In what I have read concerning this condition I have not seen the symptoms described, perhaps because the symptoms were so typical of a low blood volume. I have always wondered if they were actually treating ME.
However, there is an important point to this treatment. It does not cure the illness, even when the symptoms have been largely relieved. It makes a person feel better but there is still ‘something there’; people can get back to work or return to school, but the hypovolemia is not the primary effect of getting ME, it is a secondary effect.
There are a few other anecdotes I would like to share. I had a 38 year old man who was employed by the Navy who had developed typical moderately-severe ME. After his initial evaluation I ordered a blood volume test followed by the usual screening blood tests. His volume was about 70% of normal for his weight and sex. He was also hypertensive and very bright. As no one had been able to control his hypertension, I suggested that we might try to treat his hypertension with an infusion of saline. Any hematologist or cardiologist reading this might faint straight away, because you normally do not want to volume expand someone with hypertension, but this is a true story. The patient agreed.
He lay resting on the examining table for ½ hour while his blood pressure and pulse were recorded, roughly 180/115 blood pressure and 110 pulse even though he was not particularly nervous. One liter of saline was infused slowly while Paula took his blood pressure frequently and I paced the halls taking Valium™. The blood pressure came down to 90/60! He had ‘hypovolemic hypertension,’ meaning that because his blood volume was low, the muscles around his arteries had clamped down causing it to look like standard ‘too much blood’ hypertension. In retrospect, he remembered that diuretics made him feel worse.
Another weird anecdote: one patient with low volume and typical ME got a liter of saline and promptly fell asleep. She had a particularly bad sleep disorder with prominent insomnia, and whenever she had a saline infusion she would sleep well, with ‘restorative sleep.’ She would prefer saline to any sleeping pill available.
A third anecdote: I accompanied one patient to Dr. Streeten’s office, a patient with very prominent orthostatic intolerance. When she stood quietly she would start swaying, become confused, have excruciating pain and slur her speech. At the time Dr. Streeten was studying the effect of MAST (Military Anti-Shock Trousers) trousers on the orthostatic intolerance. These trousers, found in every ambulance, inflate with air to create a sort of total body cast for patients with fractures of the pelvis and other problems. My patient was standing quietly with the trousers in place but not inflated, and she began to have her symptom exacerbation. Dr. Streeten then inflated the trousers to 35 mm Hg, and within seven seconds she shook her head and said she felt wonderful. The slurred speech disappeared along with the pain, cognitive and other ME symptoms. Dr. Streeten published these findings[8].
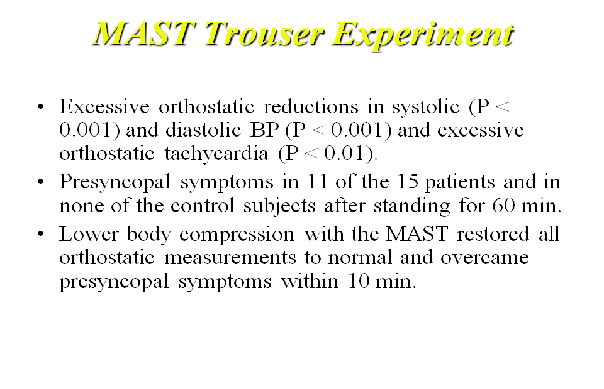
The reason this is such an important study is that the only thing the MAST trousers could have done is to improve the blood flow through the brain. Because of the instant and dramatic effect, several of my patients went and bought a set of MAST trousers, but they are not practical. Although you may feel better, you cannot do anything being encased in a whole-body cast. I have always wondered what would happen for a patient with very severe (bed-ridden) ME to have this trial.
All of this is interesting, but just a part of the 9,000 studies that have been done and forgotten in the history of ME. I think this is a shame because there is something important about the low blood volume in ME patients. And it has a cause, even though it has not been found to date. Actually, it has not been looked for, as far as I can tell.
I look forward to giving more powerpoint presentations on ME in the future, and can be reached at drdsbmd@gmail.com
David S. Bell MD
28 July 2015
- 1. Streeten DH, Thomas D, Bell DS. The roles of orthostatic hypotension, orthostatic tachycardia, and subnormal erythrocyte volume in the pathogenesis of the chronic fatigue syndrome. Am J Med Sci. 2000; 320(1): 1-8.
- 2. Hurwitz B, Coryell V, Parker M, Martin P, LaPierre A, NG K, et al. Chronic Fatigue Syndrome: illness severity, sedentary lifestyle, blood volume, and evidence of diminished cardiac function. Clin Sci. 2009.
- 3. Stewart J, Glover J, MS M. Increased plasma angiotensin II in postural tachycardia syndrome (POTS) is related to reduced blood flow and blood volume. Clin Sci. 2006; 110(2): 255-63.
- 4. Fluge O, Risa K, Lunde S, Alme K, Rekeland I, Sapkota D, et al. B-lymphocyte depletion in myalgic encephalopathy/chronic fatigue syndrome. An open-label phase II study with Rituximab maintenance treatment. PLoS ONE. 2015; 10(7).
- 5. Loebel M, Grabowski P, Heidecke H, Bauer S, Hanitsch L, Wittke K, et al. Antibodies to ß adrenergic and muscarinic cholinergic receptors in patients with Chronic Fatigue Syndrome. Brain Behav Immun. 2015.
- 6. Tanaka H, Matsuskima R, Tamai H, Kajimoto Y. Impaired postural cerebral hemodynamics in young patients with chronic fatigue syndrome with and without orthostatic intolerance. J Pediatr. 2002; 140(412-417).
- 7. Fouad F, Tadena-Thome L, Bravo E, Tarazi R. Idiopathic hypovolemia. Ann Intern Med. 1986; 104: 298-303.
- 8. Streeten D. The role of impaired lower-limb venous innervation in the pathogenesis of the chronic fatigue syndrome. Am J Med Sci. 2001; 321: 163-7.



